How antibiotic resistance in bacteria has evolved into a global threat, and discover why this growing health challenge requires urgent attention.
Antibiotic Resistance: A Growing Global Problem
Antibiotic resistance is one of the most significant public health threats today. Over the past few decades, bacteria have evolved rapidly to resist treatments that once worked well.
This resistance is happening because bacteria adapt to their environment, and when they are exposed to antibiotics repeatedly or incorrectly, they develop ways to survive.
Antibiotics that used to cure infections are now becoming less effective or, in some cases, completely useless. The implications are serious. Simple infections could become life-threatening again.
But how did bacteria become resistant to antibiotics? Let’s explore the journey and understand how this evolution took place.
The Rise of Antibiotic Use in Medicine
Antibiotics were discovered in the early 20th century, and they were considered a miracle drug. Penicillin, the first antibiotic, changed medicine. Doctors could finally treat bacterial infections that were once deadly. As the use of antibiotics became widespread, they saved millions of lives.
However, as antibiotics became more accessible, their use also became more frequent. People used them to treat all sorts of infections, sometimes even when antibiotics weren’t necessary. For instance, viral infections like colds or flu don’t respond to antibiotics, yet antibiotics were often prescribed anyway. This misuse created the perfect environment for bacteria to adapt and evolve.

As antibiotics killed off the weaker bacteria, the stronger ones, which could survive the treatment, thrived. These survivors then reproduced, passing their resistant traits to future generations. The more we used antibiotics, the faster bacteria learned how to defend themselves.
The Mechanisms Behind Resistance: How Bacteria Adapt
Bacteria have several ways to become resistant. One way is through mutations in their DNA. These changes can happen randomly, but if a mutation helps the bacteria survive antibiotic treatment, it will multiply. Over time, this resistant strain becomes dominant.
Another method is through gene transfer. Bacteria can exchange genetic material with each other. So, if one bacterium has developed resistance, it can pass that trait to other bacteria, even if they’re a different species.

This makes the spread of resistance even faster and more widespread. In hospitals, where antibiotics are heavily used, this gene transfer is particularly common.
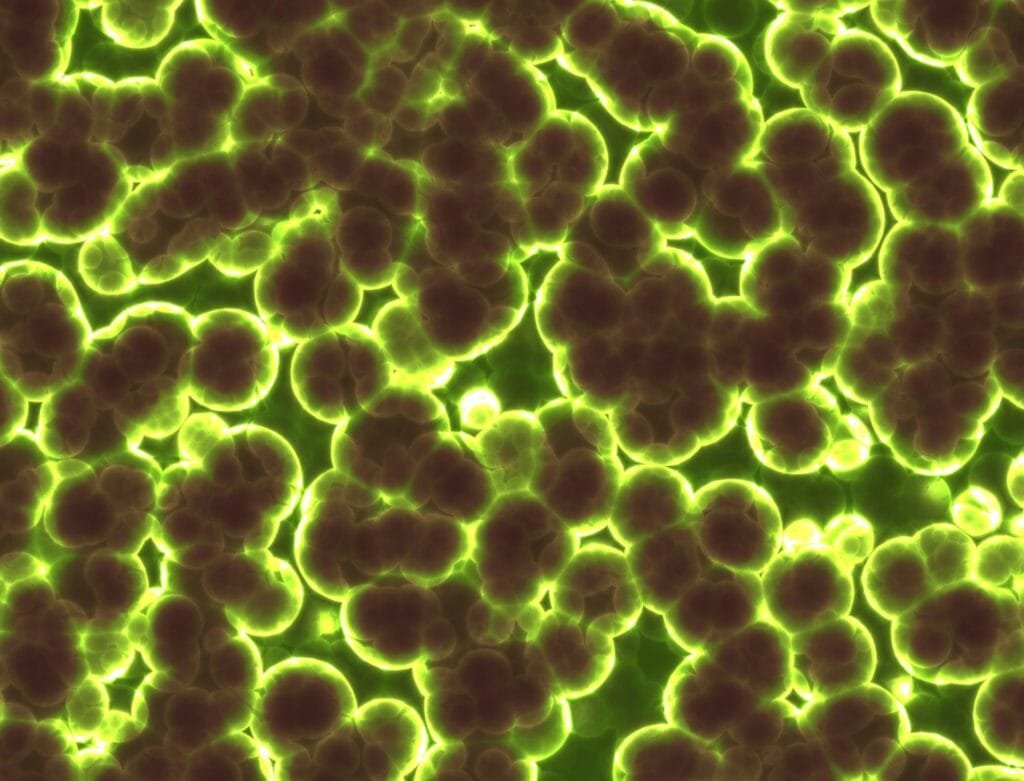
Superbugs: The Dangerous Outcome
As bacteria continue to evolve, they’ve become what we call superbugs. These are strains that are resistant to multiple types of antibiotics.
Methicillin-resistant Staphylococcus aureus (MRSA) and multidrug-resistant tuberculosis (MDR-TB) are examples of such superbugs.
Treating infections caused by these bacteria is incredibly difficult, requiring more toxic or less effective drugs. Sometimes, there are no effective treatments at all.
Infections caused by resistant bacteria can lead to longer hospital stays, higher medical costs, and more deaths.
The World Health Organization (WHO) estimates that by 2050, antibiotic-resistant infections could cause 10 million deaths per year, surpassing cancer.
Causes of Antibiotic Resistance: Overuse and Misuse
One of the main causes of antibiotic resistance is overuse. Antibiotics are often prescribed when they’re not needed, like for viral infections.
In agriculture, antibiotics are routinely given to livestock, not just to treat illness but to promote growth. This widespread use in animals contributes to resistance that can spread to humans through food.
The misuse of antibiotics is another critical factor. Many people stop taking their antibiotics early, as soon as they start feeling better, instead of finishing the full course.
This leaves some bacteria alive, which can then develop resistance. In other cases, people take leftover antibiotics or use antibiotics without a prescription, which can also lead to resistance.
The Global Impact of Antibiotic Resistance
Antibiotic resistance knows no borders. Resistant bacteria can spread from person to person, across countries, and even continents.
International travel and trade mean that a resistant infection in one part of the world can quickly become a global problem.
Low- and middle-income countries are particularly affected. In these regions, access to antibiotics is often unregulated, leading to misuse.
Poor infection control, lack of sanitation, and limited healthcare resources also make it easier for resistant bacteria to spread. This makes tackling antibiotic resistance a global issue that requires cooperation and coordination.
Fighting Back: What Can Be Done?
There are several strategies to fight antibiotic resistance:
- Judicious Use of Antibiotics
Doctors and patients need to use antibiotics more responsibly. Antibiotics should only be prescribed when absolutely necessary. Patients need to follow the full course of treatment, even if they start feeling better. - Global Policies and Regulation
Governments need to regulate the use of antibiotics, both in healthcare and in agriculture. Many countries are starting to limit the use of antibiotics in farm animals, which is a step in the right direction. - Public Education
Raising awareness about the dangers of antibiotic resistance is crucial. People need to understand why they shouldn’t misuse antibiotics and why completing their treatment is so important. - New Antibiotic Development
Pharmaceutical companies are working on developing new antibiotics, but progress is slow. One reason is that the financial incentive isn’t as strong as with other drugs. Governments and global health organizations need to provide support and funding for this research.
What the Future Holds
If we don’t act now, the future could be grim. Simple infections, which we can easily treat today, could become life-threatening again.
Surgeries and cancer treatments that rely on antibiotics to prevent infections would become riskier. We could face a future where antibiotics no longer work, leading to a post-antibiotic era.
However, there’s hope. By using antibiotics more responsibly, investing in new treatments, and raising awareness, we can slow the spread of resistance. It’s a race against time, but with global cooperation, we can protect the advances we’ve made in modern medicine.
Our Role in Fighting Antibiotic Resistance
The evolution of antibiotic resistance is a serious issue, but it’s not too late to turn the tide. By understanding how bacteria develop resistance and taking steps to prevent its spread, we can safeguard the effectiveness of antibiotics for future generations.
Whether it’s through careful use, better regulations, or innovative research, everyone has a role to play in the fight against antibiotic resistance.